Headache is one of the most common neurological complaints worldwide and a leading cause of disability. According to the World Health Organization (WHO, 2023), nearly half of adults experience at least one headache each year, and headache disorders rank among the most prevalent conditions globally. Although most headaches are not life-threatening, recurrent or severe headaches can significantly impair quality of life, occupational functioning and psychological wellbeing.
This article explores the symptoms, causes and evidence-based treatments of headaches, drawing upon textbooks, peer-reviewed journal articles and reputable health organisations using the Harvard referencing system and British spelling.
1.0 Types of Headache
Headaches are broadly classified into primary and secondary types (Olesen et al., 2018).
- Primary headaches occur independently and are not caused by another medical condition. These include:
- Tension-type headache
- Migraine
- Cluster headache
- Secondary headaches result from underlying causes such as infection, head injury, sinusitis or medication overuse (Bendtsen et al., 2018).
Understanding the type of headache is essential for appropriate management.
2.0 Symptoms of Headache
Symptoms vary depending on the specific headache disorder.
2.1 Tension-Type Headache
Tension-type headache is the most common form. According to Bendtsen et al. (2018), symptoms include:
- Dull, aching pain
- A sensation of tightness or pressure around the forehead
- Bilateral pain (both sides of the head)
- Mild to moderate intensity
- Tenderness in scalp, neck and shoulder muscles
Pain is typically not worsened by routine physical activity.
2.2 Migraine
Migraine is a neurological disorder characterised by recurrent attacks. The NHS (2023) describes typical symptoms as:
- Moderate to severe throbbing pain, often unilateral
- Nausea and vomiting
- Sensitivity to light (photophobia) and sound (phonophobia)
- Visual disturbances (aura), such as flashing lights or blind spots
For example, an individual experiencing migraine with aura may notice visual zigzag patterns before the onset of pain.
2.3 Cluster Headache
Cluster headache is less common but extremely severe. Symptoms include:
- Intense, burning or piercing pain around one eye
- Red or watery eye
- Nasal congestion
- Restlessness or agitation
Cluster headaches typically occur in cyclical patterns (May, 2018).
2.4 Red Flag Symptoms
Certain symptoms require urgent medical evaluation:
- Sudden “thunderclap headache”
- Headache following head injury
- Headache with fever, stiff neck or confusion
- Progressive worsening pattern
- New headache in individuals over 50 years
These may indicate serious conditions such as meningitis or intracranial haemorrhage.
3.0 Causes of Headache
Headaches arise from complex interactions between neurological, vascular, muscular and environmental factors.
3.1 Neurological Mechanisms
Migraine involves activation of the trigeminovascular system and release of inflammatory neuropeptides (Goadsby et al., 2017). This leads to sensitisation of pain pathways in the brain.
3.2 Muscle Tension and Posture
Poor posture and prolonged muscle contraction can contribute to tension-type headaches. Sustained contraction of neck and scalp muscles increases nociceptive signalling (Bendtsen et al., 2018).
For instance, individuals working long hours at a computer may develop neck stiffness leading to headache.
3.3 Hormonal Changes
Hormonal fluctuations, particularly oestrogen changes, can trigger migraine in women. Many report headaches linked to the menstrual cycle (MacGregor, 2017).
3.4 Stress and Psychological Factors
Stress is one of the most commonly reported headache triggers. Psychological tension may increase muscle contraction and alter neurotransmitter balance.
3.5 Environmental Triggers
Common triggers include:
- Bright lights
- Strong odours
- Loud noise
- Dehydration
- Skipped meals
- Lack of sleep
Keeping a headache diary can help identify personal triggers.
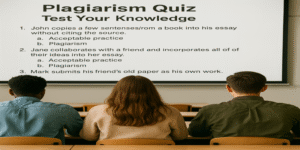
3.6 Medication Overuse
Frequent use of painkillers such as paracetamol, ibuprofen or codeine can lead to medication-overuse (rebound) headache (Olesen et al., 2018). This condition occurs when analgesics are taken more than two days per week over prolonged periods.
4.0 Treatment of Headache
Treatment depends on headache type, severity and frequency.
4.1 Acute (Abortive) Treatment
For mild to moderate headaches:
- Paracetamol
- Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen
- Aspirin
For migraine:
- Triptans, which target serotonin receptors and reduce neurovascular inflammation (Goadsby et al., 2017)
However, overuse should be avoided to prevent rebound headache.
4.2 Preventive (Prophylactic) Treatment
For frequent migraines or chronic headaches, preventive medications may include:
- Beta-blockers
- Anticonvulsants
- CGRP (calcitonin gene-related peptide) inhibitors
Preventive therapy is typically considered when headaches occur more than four times per month (NHS, 2023).
4.3 Non-Pharmacological Interventions
Lifestyle Modifications
- Regular sleep schedule
- Adequate hydration
- Balanced meals
- Regular physical activity
Exercise has been shown to reduce migraine frequency in some individuals (WHO, 2023).
Stress Management
Techniques include:
- Cognitive behavioural therapy (CBT)
- Relaxation training
- Mindfulness meditation
- Biofeedback
CBT can help modify stress-related thought patterns contributing to tension headaches.
Posture and Ergonomics
Adjusting workstation height, using supportive chairs and taking regular breaks may reduce muscle strain.
Complementary Approaches
Evidence supports limited use of:
- Peppermint oil for tension headaches
- Acupuncture
- Magnesium supplementation (for migraine prevention)
However, complementary therapies should be discussed with healthcare professionals.
5.0 When to Seek Medical Advice
Medical consultation is recommended if:
- Headaches are frequent or worsening
- Pain is severe and disabling
- Over-the-counter medication is required regularly
- Neurological symptoms accompany headache
Early diagnosis helps prevent complications and improve quality of life.
Headaches are highly prevalent and vary widely in presentation, from mild tension-type discomfort to severe migraine and cluster headaches. Symptoms may include throbbing pain, muscle tightness, nausea, light sensitivity and visual disturbances, depending on the type.
Causes are multifactorial, involving neurological mechanisms, vascular changes, muscle tension, hormonal fluctuations and environmental triggers. While acute treatment with analgesics or triptans can relieve symptoms, preventive strategies and lifestyle modifications are essential for long-term management.
Importantly, responsible medication use and recognition of red flag symptoms are crucial. With appropriate diagnosis and tailored treatment, most individuals can effectively manage headache disorders and significantly improve daily functioning.
References
Bendtsen, L., Ashina, S., Moore, R.A. and Steiner, T.J. (2018) ‘Muscle tension and tension-type headache’, The Lancet Neurology, 17(11), pp. 954–965.
Goadsby, P.J., Holland, P.R., Martins-Oliveira, M., Hoffmann, J., Schankin, C. and Akerman, S. (2017) ‘Pathophysiology of migraine: A disorder of sensory processing’, Physiological Reviews, 97(2), pp. 553–622.
MacGregor, E.A. (2017) ‘Migraine in women’, Seminars in Neurology, 37(6), pp. 601–610.
May, A. (2018) ‘Cluster headache: Pathogenesis, diagnosis, and management’, The Lancet, 381(9863), pp. 843–855.
NHS (2023) Headaches. Available at: https://www.nhs.uk/conditions/headaches/ (Accessed: 17 February 2026).
Olesen, J., Bendtsen, L., Dodick, D. et al. (2018) The International Classification of Headache Disorders (ICHD-3). 3rd edn. Cephalalgia, 38(1), pp. 1–211.
World Health Organization (WHO) (2023) Headache disorders. Available at: https://www.who.int/news-room/fact-sheets/detail/headache-disorders (Accessed: 17 February 2026).