Stakeholder analysis and engagement are critical to the success of organisational change initiatives. Stakeholders are individuals or groups with a vested interest in, or influence over, a project, programme, or transformation (Freeman, 1984). Their perceptions, expectations, and levels of support or resistance significantly affect outcomes. By systematically analysing stakeholders, managers can identify power dynamics, interests, and potential areas of resistance, enabling the design of tailored strategies to foster alignment. Equally important, engaging stakeholders through inclusive participation, co-design, and communication builds legitimacy, ownership, and commitment to change. This article examines theories, practices, and real-world applications of stakeholder analysis and engagement, with particular reference to healthcare digitalisation and corporate transformation.
Stakeholder Analysis: Frameworks and Tools
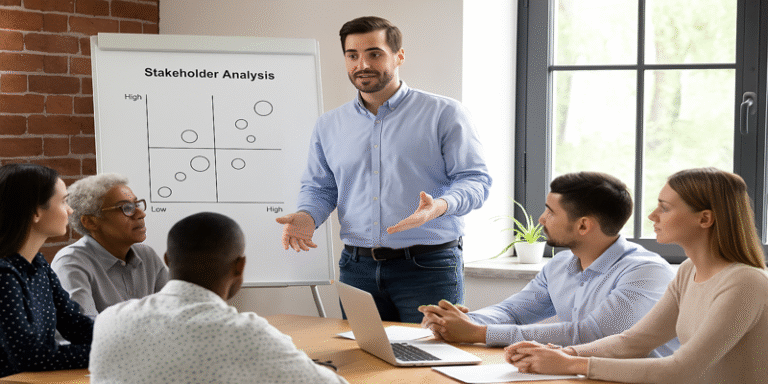
Stakeholder analysis involves identifying, categorising, and prioritising stakeholders. A widely cited model is the power-interest matrix, which maps stakeholders by their influence over, and interest in, a change initiative (Cameron and Green, 2015). Those with high power and high interest must be engaged closely, while those with low power and low interest may require minimal attention.
Mitchell, Agle and Wood (1997) developed the salience model, which evaluates stakeholders based on power, legitimacy, and urgency. This helps organisations prioritise which stakeholders to address first, especially under resource constraints. Similarly, Scholes and Clutterbuck (1998) highlight the importance of identifying opinion leaders within stakeholder networks, as these actors can either accelerate or block acceptance of change.
In corporate practice, Unilever’s Sustainable Living Plan demonstrated how structured stakeholder mapping across regulators, investors, employees, and NGOs enabled the company to balance conflicting demands while securing broad legitimacy (Unilever, 2019). By anticipating stakeholder concerns, Unilever avoided reputational risks and embedded sustainability within its business model.
Stakeholder Engagement: From Communication to Co-Creation
Stakeholder engagement extends beyond consultation to include co-design and co-creation. Traditional approaches often relied on one-way communication, where leaders disseminated information to stakeholders. However, contemporary perspectives stress dialogue, participation, and empowerment (Greenhalgh et al., 2016). Engagement is now seen as a relational process where stakeholders co-create value, knowledge, and solutions.
Recent scholarship emphasises healthcare digitalisation as a prime context for stakeholder engagement. For example, Laurisz et al. (2023) found that involving clinicians, patients, and managers in co-creating digital services under the “Healthcare 4.0” paradigm led to greater adoption rates and sustainability. Similarly, Wentzel, Van Limburg and Karreman (2012) showed that co-creation in antibiotic stewardship programmes increased compliance and reduced resistance from medical staff.
Corporate examples further illustrate this. Microsoft’s transformation under Satya Nadella involved engaging employees as change partners, not just recipients. By promoting a growth mindset and inclusive dialogue, the company overcame cultural resistance and achieved sustained performance gains (Takahashi and Takahashi, 2022).
Stakeholder Engagement in Healthcare: Co-Creation in Action
Healthcare is increasingly shaped by multi-stakeholder ecosystems where patients, providers, regulators, and technology companies intersect. Engagement is essential to navigate this complexity. Claessens et al. (2022) proposed a co-creation roadmap for sustainable healthcare quality, highlighting the need for early involvement of clinicians to avoid implementation failures. Similarly, Tončinić et al. (2020) evaluated digital platforms enabling patients, clinicians, and researchers to co-design healthcare innovations, demonstrating enhanced usability and acceptance.
Digital transformation initiatives often fail when frontline clinicians feel excluded. Garmann-Johnsen, Helmersen and Eikebrokk (2018) showed that web 2.0 tools enabling staff contributions fostered ownership of digital change processes. This is consistent with Janamian and Crossland (2016), who developed a framework for value co-creation in primary care, stressing patient inclusion in service design.
Beyond adoption, engagement fosters trust. In vaccine development and distribution, engaging communities through transparent dialogue reduced hesitancy and built public trust in science (Best, Moffett and McAdam, 2019). This example shows that co-production of legitimacy is as important as technical success.
Corporate Transformation and Stakeholder Legitimacy
In the corporate sector, stakeholder engagement enhances legitimacy during major transformations. Unilever, as noted, engaged NGOs and consumers in shaping its sustainability strategy. Similarly, Schiavone, Leone and Sorrentino (2020) demonstrated that co-creation in healthcare networks improved service experiences and stakeholder satisfaction. By analogy, corporations engaging customers in product innovation co-create shared value and reduce resistance.
Large-scale digital business models in healthcare and beyond require engaging multiple stakeholders simultaneously. Schiavone, Mancini and Leone (2021) described how ridesharing-based healthcare models required alignment between patients, regulators, and service providers to function effectively. Without active engagement, conflicting interests could stall innovation.
Challenges and Limitations
While beneficial, stakeholder engagement poses challenges. First, it can be time-consuming and resource-intensive (Greenhalgh et al., 2016). Achieving consensus among diverse stakeholders may delay implementation. Second, power imbalances can marginalise certain voices, particularly patients in healthcare or lower-level employees in corporations (Aflaki and Lindh, 2023). To mitigate this, managers must ensure equitable participation mechanisms.
Third, engagement without genuine influence risks tokenism. Stakeholders may feel disillusioned if their input does not affect outcomes (Carlini et al., 2024). Therefore, transparency about the scope of influence is vital. Finally, engagement must adapt to cultural contexts. What works in a European healthcare system may not translate directly to Asian or African contexts due to differing stakeholder expectations and power structures (Nudurupati et al., 2015).
Effective stakeholder analysis and engagement are indispensable for change success. By mapping power, interest, and salience, managers can anticipate resistance and design responsive strategies. By moving from consultation to co-creation, organisations foster trust, legitimacy, and adoption. Evidence from healthcare digitalisation demonstrates how engaging clinicians, patients, and policymakers increases sustainability, while corporate cases such as Unilever illustrate the strategic value of inclusive engagement in building legitimacy. Nevertheless, challenges such as resource constraints, power imbalances, and risks of tokenism require careful management. Ultimately, stakeholder engagement is not just a management tool but a governance imperative for sustainable transformation in both healthcare and corporate contexts.
References
Aflaki, I.N. and Lindh, M. (2023). Empowering first-line managers as change leaders towards co-creation culture: the role of facilitated sensemaking. Public Money & Management. https://doi.org/10.1080/09540962.2021.2007636.
Best, B., Moffett, S. and McAdam, R. (2019). Stakeholder salience in public sector value co-creation. Public Management Review, 21(11), pp.1595–1615.
Cameron, E. and Green, M. (2015). Making Sense of Change Management. 4th ed. Kogan Page.
Carlini, J., Muir, R. and McLaren-Kennedy, A. (2024). Transforming health-care service through consumer co-creation. Journal of Services Marketing, 38(2), pp.221–237.
Claessens, F., Seys, D., Brouwers, J. and Van Wilder, A. (2022). A co-creation roadmap towards sustainable quality of care. PLoS ONE, 17(6), e0269364.
Freeman, R.E. (1984). Strategic Management: A Stakeholder Approach. Pitman.
Garmann-Johnsen, N.F., Helmersen, M. and Eikebrokk, T.R. (2018). Digital transformation in healthcare: enabling employee co-creation through web 2.0. AMCIS Proceedings.
Greenhalgh, T., Jackson, C., Shaw, S. and Janamian, T. (2016). Achieving research impact through co‐creation. The Milbank Quarterly, 94(2), pp.392–429.
Janamian, T. and Crossland, L. (2016). Embracing value co‐creation in primary care services research. Medical Journal of Australia, 204(7), pp. S7–S10.
Laurisz, N., Ćwiklicki, M., Żabiński, M. and Canestrino, R. (2023). Co-creation in Health 4.0 as a new solution for a new era. Healthcare, 11(3), 363.
Mitchell, R.K., Agle, B.R. and Wood, D.J. (1997). Toward a theory of stakeholder identification and salience. Academy of Management Review, 22(4), pp.853–886.
Schiavone, F., Leone, D. and Sorrentino, A. (2020). Re-designing the service experience in the value co-creation process. Business Process Management Journal, 26(3), pp.601–619.
Schiavone, F., Mancini, D. and Leone, D. (2021). Digital business models and ridesharing for value co-creation in healthcare. Technological Forecasting and Social Change, 166, 120639.
Takahashi, S. and Takahashi, V.P. (2022). Analysis of front-end dynamics in value co-creation with multiple stakeholders. International Journal of Managing Projects in Business, 15(5), pp.742–760.
Unilever (2019). Unilever Sustainable Living Plan. https://www.unilever.com/sustainable-living/.
Wentzel, J., Van Limburg, M. and Karreman, J. (2012). Co-creation with stakeholders: A web 2.0 antibiotic stewardship program. Proceedings of eTelemed 2012.