The cardiovascular system plays a vital role in maintaining homeostasis by ensuring the effective transport of oxygen, nutrients, and waste products. Central to this system are three closely related physiological parameters: blood pressure, pulse rate, and heart rate. Although these terms are sometimes used interchangeably in lay discussions, they represent distinct but interlinked aspects of cardiovascular function. Understanding their physiology and clinical significance is essential not only for healthcare practitioners but also for individuals monitoring their health.
1.0 Blood Pressure
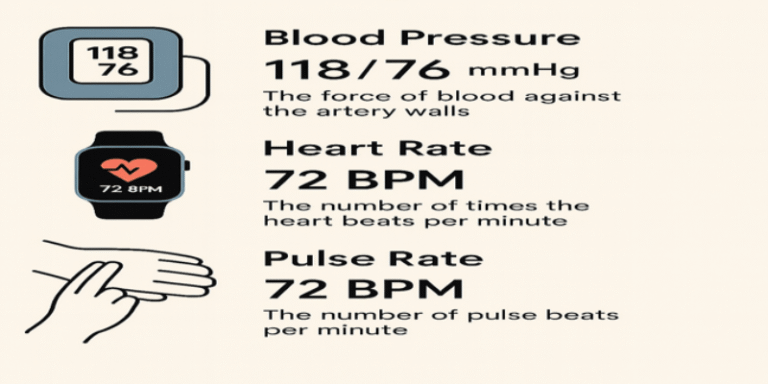
Blood pressure (BP) is defined as the force exerted by circulating blood on the walls of blood vessels, particularly arteries. It is measured in millimetres of mercury (mmHg) and expressed using two values: systolic pressure, which occurs during heart contraction, and diastolic pressure, measured during heart relaxation (Marieb and Hoehn, 2019). A typical normal adult BP reading is around 120/80 mmHg.
BP is regulated through complex mechanisms involving cardiac output, vascular resistance, blood volume, and neurohormonal responses (Hall and Guyton, 2020). The autonomic nervous system plays a critical role in short-term regulation, while the renal system and endocrine factors such as the renin-angiotensin-aldosterone system (RAAS) contribute to long-term control (Klabunde, 2012).
2.0 Pulse Rate and Heart Rate: A Distinction
Heart rate (HR) refers to the number of times the heart beats per minute (bpm), while the pulse rate is the number of palpable pulses detected in a peripheral artery, usually matching the HR under normal conditions (Moorhead and Cook, 2020). However, in conditions such as arrhythmias or atrial fibrillation, the pulse rate may not accurately reflect the true heart rate due to irregular ventricular responses.
Pulse is typically measured manually at the radial artery, while heart rate can be assessed more accurately using electrocardiography (ECG) or photoplethysmographic sensors, such as those in modern wearable devices like the Apple Watch (Zhang et al., 2019).
3.0 Normal Ranges and Variability
For healthy adults, the following ranges are generally considered normal:
- Blood Pressure: 90/60 mmHg to 120/80 mmHg
- Resting Heart Rate: 60–100 bpm
- Pulse Rate: Usually equal to heart rate unless in arrhythmia
Factors influencing these values include age, sex, fitness level, body size, emotional state, and medications (NICE, 2019).
4.0 Physiological and Pathological Influences
4.1 Exercise and Activity
During physical exertion, HR and BP increase to meet the elevated oxygen demand of muscles. This is a normal physiological response. After exercise, HR and BP return to baseline, and the speed of this recovery can be a marker of cardiovascular fitness (Thompson et al., 2010).
4.2 Stress and Hormonal Influences
Emotional stress stimulates the sympathetic nervous system, increasing HR and BP via adrenaline release. Chronic stress can contribute to hypertension and cardiovascular disease (Dimsdale, 2008).
4.3 Pathological Conditions
- Hypertension: Persistent elevation of BP above 140/90 mmHg is associated with increased risk of stroke, myocardial infarction, and renal failure (WHO, 2023).
- Bradycardia: HR below 60 bpm, which may be normal in athletes but pathological in others.
- Tachycardia: HR above 100 bpm at rest can indicate fever, anaemia, or cardiovascular abnormalities.
5.0 Monitoring Tools and Technology
Advancements in technology have enabled non-invasive, continuous monitoring of HR and BP. Devices such as automated blood pressure monitors, wearable fitness trackers, and smartwatches utilise sensors and algorithms to estimate physiological parameters (Shcherbina et al., 2017). The Apple Watch, for example, uses photoplethysmography to detect changes in blood volume and estimate HR (Apple, 2024).
While convenient, wearable devices may lack the precision of clinical-grade equipment and are best used for trend analysis rather than diagnostic purposes (Bent et al., 2021).
6.0 Clinical Importance
Accurate measurement and interpretation of BP, HR, and pulse are critical for diagnosing and managing cardiovascular disorders. For instance:
- Elevated BP can suggest hypertension, requiring lifestyle changes or pharmacotherapy.
- Irregular pulse may indicate arrhythmias, such as atrial fibrillation, which increases the risk of stroke.
- Monitoring HR is essential in exercise prescription, particularly for cardiac rehabilitation patients.
In primary care, these metrics are essential screening tools, while in intensive care units, they are continuously monitored for acute changes in patient status (Peate and Nair, 2017).
7.0 Public Health Implications
Hypertension affects over 1.28 billion adults worldwide and is a major risk factor for premature death (WHO, 2023). Regular monitoring of BP and HR enables early intervention, potentially reducing morbidity and mortality.
Government and health agencies recommend routine checks, particularly in at-risk populations. The UK National Health Service (NHS) encourages adults over 40 to have their BP checked at least every five years (NHS, 2022).
Understanding the interplay between blood pressure, pulse rate, and heart rate is fundamental to cardiovascular physiology and health monitoring. These parameters offer insights into the heart’s function, vascular health, and systemic balance. Whether measured manually or via modern wearable technology, they serve as critical indicators for clinical assessment, disease prevention, and personal health management.
Ongoing public education and the use of reliable monitoring tools are essential to empower individuals and reduce the global burden of cardiovascular diseases.
References
Apple (2024) Heart rate notifications and Apple Watch. Available at: https://support.apple.com/en-gb/HT208931 (Accessed: 20 July 2025).
Bent, B. et al. (2021) ‘Investigating sources of inaccuracy in wearable optical heart rate sensors’, NPJ Digital Medicine, 4(1), pp. 1–9. https://doi.org/10.1038/s41746-021-00421-8
Dimsdale, J.E. (2008) ‘Psychological stress and cardiovascular disease’, Journal of the American College of Cardiology, 51(13), pp. 1237–1246.
Hall, J.E. and Guyton, A.C. (2020) Guyton and Hall Textbook of Medical Physiology. 14th edn. Philadelphia: Elsevier.
Klabunde, R.E. (2012) Cardiovascular Physiology Concepts. 2nd edn. Philadelphia: Lippincott Williams & Wilkins.
Marieb, E.N. and Hoehn, K. (2019) Human Anatomy & Physiology. 11th edn. Harlow: Pearson.
Moorhead, S. and Cook, N. (2020) Vital Signs for Nurses: An Introduction to Clinical Observations. 2nd edn. Chichester: Wiley-Blackwell.
NHS (2022) Check your blood pressure. Available at: https://www.nhs.uk/conditions/blood-pressure-test/ (Accessed: 20 July 2025).
NICE (2019) Hypertension in adults: diagnosis and management. NICE guideline [NG136]. Available at: https://www.nice.org.uk/guidance/ng136 (Accessed: 20 July 2025).
Peate, I. and Nair, M. (2017) Fundamentals of Anatomy and Physiology for Nursing and Healthcare Students. 2nd edn. Chichester: Wiley-Blackwell.
Shcherbina, A. et al. (2017) ‘Accuracy in wrist-worn, sensor-based measurements of heart rate and energy expenditure in a diverse cohort’, Journal of Personalized Medicine, 7(2), p. 3.
Thompson, P.D. et al. (2010) ‘Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease’, Circulation, 107(24), pp. 3109–3116.
World Health Organization (WHO) (2023) Hypertension. Available at: https://www.who.int/news-room/fact-sheets/detail/hypertension (Accessed: 20 July 2025).
Zhang, Z. et al. (2019) ‘Photoplethysmography for wearable biometric measurements and human health monitoring’, Journal of Biomedical Optics, 24(1), p. 1.